SCMA Checklist: How Should Medical Waste Be Treated?
By SCMA On 11/01/2017


Along with the need to juggle admin roles and responsibilities, among the concerns medical assistants have to stay on top of is minimizing the risk of transmission-based diseases like Hepatitis and HIV in the clinic.
In supporting physicians while providing comprehensive care to patients, there are many simple processes like proper sterilization, disinfection and isolation precautions that have to be given premium importance. One of the easily neglected of these precautions is proper biomedical segregation.
The United States Environmental Protection Agency (EPA) has compiled some FAQ'S which can help to understand the importance of biomedical waste management in healthcare.
What is Medical Waste?
Medical waste is a subset of wastes generated at health care facilities, such as hospitals, physicians' offices, dental practices, blood banks, and veterinary hospitals/clinics, as well as medical research facilities and laboratories. Generally, medical waste is healthcare waste that that may be contaminated by blood, body fluids or other potentially infectious materials and is often referred to as regulated medical waste.
Why is it important to treat medical waste?
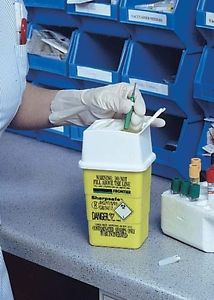
Improper management of discarded needles and other sharps can pose a health risk to the public and waste workers. For example, discarded needles may expose waste workers to potential needle stick injuries and potential infection when containers break open inside garbage trucks or needles are mistakenly sent to recycling facilities. Medsharps Compliance Portal stresses that janitors and housekeepers also risk injury if loose sharps poke through plastic garbage bags. Used needles can transmit serious diseases, such as human immunodeficiency virus (HIV) and hepatitis.
What are the types of medical waste?
- Sharps - The American Board Resources Association defines sharps as objects or devices having acute rigid corners, edges, proturbances capable of cutting or piercing (American Blood Resources Association 1986).These include hypodermic needles, syringes, scalpel blades etc. The potential for infection from contact with Medical Waste sharps is significantly greater than related to contact with non sharp waster.
- Cultures and Stocks - These wastes from Pathological and medical laboratory have high potential for transmission.
- Bulk Human Blood and Blood Products - These include blood, serum, plasma and other blood components.
- Pathological Waste - This includes Human tissues, organs, body parts and body fluids removed during surgery.
- Isolation Wastes - Includes wastes contaminated with blood, excretions,exudates or secretions from sources isolated to protect others from highly communicable infectious diseases.
- Animal Wastes – Contaminated animal caracasses, body parts, fluids and beddings of animals that have been afflicted by zoonotic diseases etc.
- Unused Sharps - Although much less likely to cause disease upon injury, their remains the risk of physical injury.
- Others include low level radioactive waste from medical institutions, antineoplastics and chemical wastes.
How should medical waste be treated?
More than 90 percent of potentially infectious medical waste in the United States was incinerated before 1997. In August of 1997, EPA (United States Environmental Protection Agency) promulgated regulations creating stringent emission standards for medical waste incinerators due to significant concerns over detrimental air quality affecting human health.
Here are the EPA's potential alternatives to incineration of medical waste:
• Thermal treatment, such as microwave technologies;
• Steam sterilization, such as autoclaving;
• Electropyrolysis; and
• Chemical mechanical systems, among others.
How do we manage medical waste?
1. Basic principles of management are listed below
• Ascertain which hazards are present in each waste.
• Assess the relative degree of risk present in each hazard.
• Assign priority to hazard with greater risk
• Develop a management scheme based on relative degrees of risk.
2. Select treatment management procedures that are compatible with all hazards present in waste.
3. If possible select a treatment technique that will provide suitable treatment for all hazards.
4. If necessary provide additional treatment for eliminating remaining hazards.
If necessary provide additional treatment for eliminating remaining hazards.
Minimization - The shift to use of disposable products for healthcare and implementation of universal precautions has significantly increased quantity of medical waste.
 844.885.1476
844.885.1476
